Dry socket, also called alveolar osteitis, is one of the most common complications that can occur after a tooth extraction, especially after the removal of wisdom teeth. It happens when the protective blood clot at the extraction site is dislodged or fails to form, leaving the bone and nerves exposed and causing significant pain. This condition may affect up to 30 percent of patients after wisdom tooth surgery and can slow the healing process if not treated promptly. In this guide, we explain the symptoms, causes, prevention tips, and treatment options for dry socket.
What Is Dry Socket?
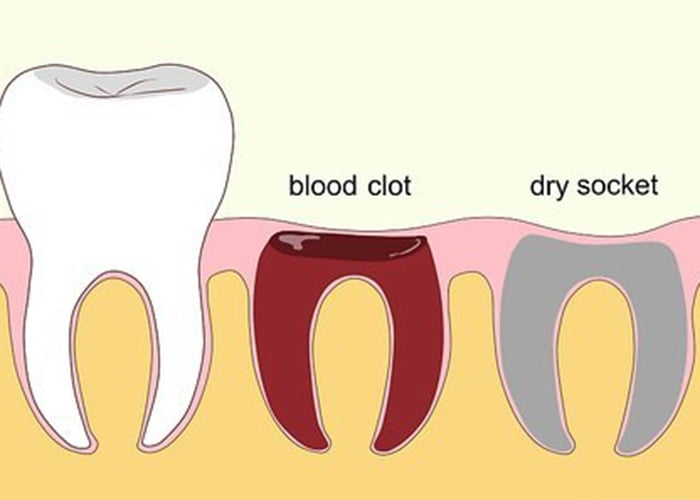
Dry socket, also called alveolar osteitis, is a painful complication that can occur after a tooth is extracted. Normally, a blood clot forms in the empty socket to protect the bone and nerves underneath. This clot is made up of blood cells and natural healing agents that reduce pain, prevent infection, and support tissue regeneration.
According to the Mayo Clinic, a dry socket happens when the blood clot either dissolves too soon or never forms at all. As a result, the socket remains open and exposed to air, food particles, and bacteria. This can cause sharp, throbbing pain that often begins two to three days after the extraction and may radiate toward the ear, temple, or neck.
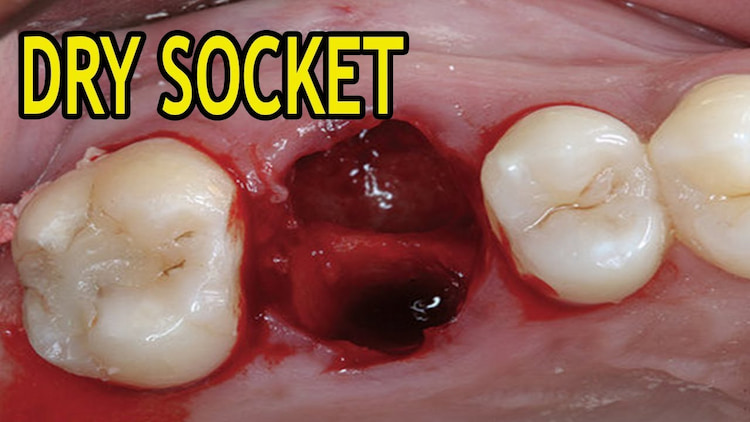
In most cases, the exposed socket appears white because of visible bone. It may also look dry or have a bad odor. If infection sets in, other signs like swelling, a foul taste, or mild fever may follow. While dry socket is not common, it tends to occur more often after wisdom tooth removal or complicated extractions.
Without treatment, the pain can last for several days and interfere with healing. This is why it’s important to recognize the symptoms early and contact your dentist if you suspect something is wrong.
Common Dry Socket Symptoms
Here’s a quick overview of the most reported dry socket symptoms, also known as alveolar osteitis, and what each one means for your recovery after a tooth extraction:
| Symptom | What It Means |
|---|---|
| Throbbing or intense pain | Pain usually begins two to four days after the extraction and may radiate to the jaw, ear, temple, or neck on the affected side. It often feels deeper and sharper than normal post-extraction pain. |
| Visible bone at the extraction site | The empty socket appears white or gray due to exposed bone, indicating that the protective blood clot is missing. This is the most telltale sign of a dry socket. |
| Bad breath or unpleasant taste | Patients often report a foul smell or metallic taste coming from the extraction site. This happens due to trapped food debris or early bacterial buildup. |
| Delayed or abnormal healing | The socket may look dry or unfilled compared to a normal healing socket. The surrounding gum tissue may appear pale, irritated, or inflamed. |
| Swollen lymph nodes or low-grade fever | In some cases, patients may experience swelling near the jaw, mild fever, or general discomfort. These symptoms may suggest early infection or prolonged inflammation. |
What Causes a Dry Socket?
Dry socket can result from several biological, lifestyle, and procedural factors that interfere with the blood clot’s formation or stability after a tooth extraction. Recognizing these risks can help prevent complications:
- Smoking or tobacco use: Nicotine reduces blood flow and interferes with healing.
- Poor post-operative oral hygiene: Increases the risk of bacterial contamination and clot displacement.
- Early rinsing, spitting, or straw use: Creates suction or pressure that may dislodge the clot.
- Hormonal factors: Estrogen fluctuations from oral contraceptives may influence healing.
- Local infections: Active gum disease or infections at the extraction site can impair blood clot stability.
- Previous dry socket history: Patients who have had dry socket before are more likely to develop it again.
- Medications: Blood thinners, corticosteroids, and antidepressants may interfere with clotting or immune response.
- Systemic health conditions: Chronic illnesses like diabetes, thyroid disorders, and autoimmune diseases can impair wound healing and tissue regeneration.
Understanding these causes allows patients to take proactive steps toward a smoother recovery and helps dental providers create tailored aftercare plans.
Worried about pain after a tooth extraction?
If you think you might have a dry socket or just want peace of mind, don’t wait. Contact Smile Plus Dentistry today for expert advice and prompt care that puts your comfort first.
How to Reduce the Risk of Dry Socket
Reducing your risk of dry socket begins with mindful care in the first few days after a tooth extraction. The following tips support the healing process and help protect the surgical site:
| Prevention Tip | Why It Matters |
|---|---|
| Avoid disturbing the clot | Refrain from smoking, drinking through a straw, spitting, or rinsing forcefully. |
| Apply firm but gentle pressure | Bite on the gauze as instructed to help the clot form and stabilize. |
| Stick to soft, bland foods | Eat items like yogurt, mashed potatoes, and soups that will not irritate the site. |
| Practice careful hygiene | Use saltwater rinses after 24 hours and avoid brushing directly over the socket. |
| Stay well hydrated and rest | Hydration and sleep promote proper immune response and tissue repair. |
Additional recommendations include avoiding alcohol, limiting physical activity in the first 24 hours, and following your dentist’s specific aftercare instructions. If you are experiencing unusual pain or complications, you can receive emergency dental care for immediate help. If you are at higher risk due to certain health conditions or medications, speak with your provider about personalized precautions to support safe healing.

Treatment Options for Dry Socket
Effective management of dry socket, or alveolar osteitis, involves a combination of in-office procedures and at-home care to alleviate pain and promote healing. The following treatments are commonly employed:
1. Socket Irrigation
Gently flushing the socket with sterile saline or an antimicrobial solution, such as chlorhexidine gluconate, helps remove food particles and bacterial debris. This process reduces irritation and lowers the risk of secondary infection.
2. Medicated Dressings
After irrigation, a dentist may place a medicated dressing into the socket. Materials like Alvogyl™, which contain eugenol, provide analgesic and anti-inflammatory effects. These dressings are typically changed every 24 to 48 hours until symptoms subside.
3. Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are commonly recommended to manage pain and inflammation. In cases of severe discomfort, a dentist might prescribe stronger analgesics.
4. At-Home Care
Patients are advised to rinse gently with warm salt water starting 24 hours after the procedure. Maintaining good oral hygiene, staying hydrated, and knowing how to brush properly after tooth removal all help protect the blood clot and reduce the risk of dry socket.
5. Follow-Up Appointments
Regular dental check-ups ensure that the socket is healing properly. If symptoms persist beyond a few days, further evaluation may be necessary to rule out complications.
By adhering to these treatment protocols, patients can expect relief from dry socket symptoms and a return to normal healing within a week or two.
Conclusion
Dry socket is one of the most uncomfortable complications after tooth extraction, but with the right care and timely treatment, it can be managed effectively. Knowing the symptoms, following your aftercare instructions, and seeking help early can make a big difference in your recovery. If you’re experiencing intense pain or suspect something isn’t healing properly, it’s always best to get it checked.
Regular dental checkups help identify potential risks before a tooth extraction and support proper healing afterward. Discover how a dental checkup in Surrey can reduce your chances of complications like dry socket.
FAQs:
How do I know if I have a dry socket or just normal post-extraction pain?
It’s completely normal to feel some pain after a tooth is removed. But if that pain suddenly gets worse around day three or four, and spreads to your ear, neck, or temple, it may be a dry socket. You might also notice a bad taste or smell in your mouth, or even see the bone where the tooth was. If this sounds familiar, it’s important to get in touch with us so we can check and help you heal faster.
Can I still eat if I have a dry socket?
Yes, but you’ll need to be careful. Choose soft foods that do not require much chewing, such as yogurt, mashed potatoes, or oatmeal. Avoid anything crunchy, spicy, or hot that might irritate the area. If you need help planning your meals during recovery, we are happy to give you personalized suggestions.
Can mouthwash prevent dry socket?
Mouthwash alone does not prevent dry socket and may even dislodge the healing clot if used too early. Avoid any rinsing for the first 24 hours. After that, only use alcohol-free or dentist-recommended rinses to support healing gently.
Does salt water prevent dry sockets?
Salt water helps keep the extraction site clean and may reduce bacteria, but it does not guarantee dry socket prevention. Begin rinsing gently with warm salt water 24 hours after extraction to support healing and avoid disrupting the blood clot.
When can I stop worrying about getting dry socket?
The risk of dry socket is highest during the first few days after a tooth extraction, especially between days three and five. After the first week, the chances drop sharply. Still, it’s important to continue following proper care instructions.
Does throbbing pain always mean dry socket?
Not always. Mild throbbing is normal after extraction. However, intense, deep, or worsening pain starting two to four days later may signal a dry socket, especially if accompanied by visible bone, bad taste, or no improvement with pain medication.
Have you experienced a dry socket before, or do you have questions about your recovery? Share your thoughts or ask your questions in the comments below. We’d love to hear from you.

No Comments